I’ve got Polymyalgia Rheumatica, I will recover!
- Zsuzsanna Schmidt
- Oct 6, 2018
- 3 min read
Updated: Apr 12, 2025
„I have intense pains in my shoulders and I cannot elevate my arms! It takes many hours just to feel slightly better. I have malaise and probably some fever... and my knees are swollen, look! I am 60 years old. Until now I had had no health problems, and I do not feel that I am old enough to have such bad pain and discomfort. When I went to the GP, he took my blood sample and guess what; my ESR was extremely high, 100 mm/h! What is wrong with me? What on earth is this disease that I have?”
...ask my patients, who are actually suffering from a relatively frequent disease of the “elderly” called polymyalgia rheumatica.
Polymyalgia rheumatica (PMR) - despite its name - is in fact an articular disease, not a muscular disease. It is an inflammatory disease. Although locomotor symptoms feature, it is a disease of the whole body. Musculoskeletal symptoms are characterised by pain, aching and morning stiffness in the shoulder girdle and often hip girdle and neck. Prolonged morning stiffness lasts for hours or all day long. Constitutional symptoms, fatigue, malaise, weight loss and low grade fever may also be associated. Marked systemic inflammation with high ESR and CRP values are characteristic and rapid response to corticosteroid (CS) therapy is generally observed. Giant cell arteritis is a well-known association of PMR, both are diseases of the elderly, aged 50 years or over.

PMR (with associating arteritis) in the art
„Archbishop of van der Paele” Jan van Eyck 1436, Bruges
Although the characteristic, non-specific proximal syndrome predominates, less well recognizable and more variable distal musculoskeletal manifestations can also be observed, asymmetric lower extremity oligoarthritis with knee involvement, tenosynovitis of the hands and feet, and carpal tunnel syndrome. Remitting symmetric pitting edema of the hands is also a characteristic phenomenon in the elderly.

Typical picture of a PMR patient, because of the intense pain she is not able to elevate her arms
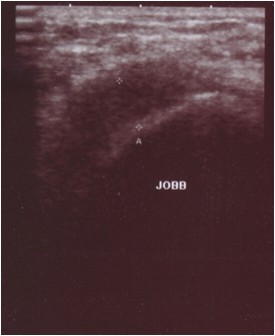
Pathology of the locomotor system can be visualised by modern imaging. MR and US show mild, non-erosive synovitis, with marked inflammation of the extraarticular synovial structures, bursitis and tenosynovitis. Hence the diffuse periarticular pain of the shoulders and hips.
MRI and US of the PMR patient, bursitis and tenosynovitis
As there is no pathognostic sign, PMR diagnosis starts with its differentiation from polymyalgia mimics; the emphasis being on elderly onset inflammatory arthritides. Elderly onset rheumatoid arthritis (RA) may start with shoulder involvement, but symmetric hand polyarthritis predominates. Without treatment, polyarthritis leads to destruction of joints, and the well known deformities of RA. Late onset seronegative spondylarthritis may also start with bilateral shoulder complaints, but the sacroiliac features help to differentiate. Differentiation from malignancies and chronic infections should also be emphasized, constitutional symptoms, weight loss and fever are characteristic.
PMR diagnosis is based on the typical clinical features. The old diagnostic criteria were related to the experience of outstanding experts of the field. New classification criteria, 2012 were elaborated by the international PMR work group under the aegis of the American and European Rheumatology Associations, the scoring algorythm of which is also based on clinical symptoms.
Corticosteroids remain the cornerstone of PMR therapy, no effective steroid-sparing drug has been found to date. CSs are generally needed for 1-1.5 years. Despite the serious beginning of the disease, the majority of patients recover. Cautious and gradual decreasing of the CS dose is very important. In a symptom-free patient taking GCs the inflammation continues. The risk for relapse is higher if CS therapy has been decreased or stopped before the appropriate time. In the case of a correct therapy scheme it may also occur that some patients have a chronic-relapsing course and require CSs for several years. Steroid-related side effects are well-known (weight gain and obesity, diabetes, hypertension, hyperlipidaemia and osteoporosis). For steroid-sparing many of the DMARDs, which work in different arthritides, have been tried without much success. In the case of a relapse, methotrexate and leflunomide should be introduced.
Early recognition of the disease, early start and well-defined course of CS therapy, prevention and management of its side effects are every day tasks for rheumatologists and family doctors. Follow-up of PMR patients after their recovery is also essential.